One of the sounds that no one enjoys hearing is a bed partner snoring. However, that piercing, rasping sound could sometimes be more than just a nuisance. About half of the 90 million snorers in Australia have obstructed sleep apnea (OSA), a problem that seriously impairs breathing, is linked to heart disease, and may even be fatal. Furthermore, you may not even be conscious of having the disease.
Unsurprisingly, many people don’t get therapy for snoring
Unsurprisingly, many people don’t get therapy for snoring because they don’t see it as a severe issue. Or they do, but they decline to take part in a 24-hour lab sleep test (which is how sleep apnea is typically diagnosed). Or they worry that if they are diagnosed with OSA, they will have to use the most well-known and notoriously painful kind of treatment: a CPAP machine.
In addition, a growing number of OSA sufferers are unsure if they really need to use a CPAP since a company recently had to recall some of its CPAP devices.
In order to clear out the confusion, we sought the advice of Yale’s Center for Sleep Medicine director Henry Yaggi, MD, MPH, a pulmonologist, and Andrey Zinchuk, MD, MHS, the director of Yale’s Advanced Apnea Management Program.
They collaborated with us to come up with a list of the top seven facts about CPAP technology improvements, alternative OSA treatments, and obstructive sleep apnea.
1. Obstructive sleep apnea
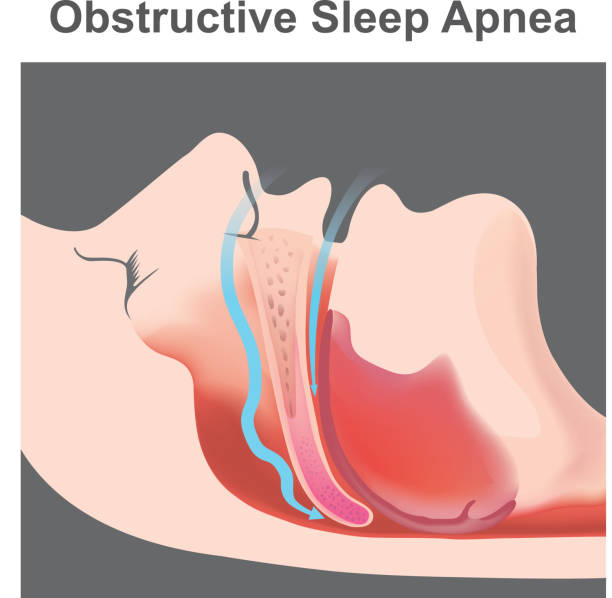
Obstructive sleep apnea is the most common kind of sleep apnea, in which your breathing periodically stops and restarts while you are sleeping. Additionally, central apnea develops when the brain mismanages respiratory regulation. and mixed apneas, which blend obstructive and central apneas.
The muscles at the back of your throat relax while you sleep, which increases the likelihood that OSA-related constriction or closure may occur. While you’re sleeping, you could snore, snort, or make other noises while you try to breathe. As a result of the air loss, your blood oxygen level may decrease, which might prompt your brain to signal for you to get up.
Whether or not they are aware of it, some OSA patients experience hundreds of episodes of stopped or interrupted breathing each night, and this may have a substantial detrimental impact on their quality of life throughout the day.
2. Improvements have been made to CPAP machines.
a brief history The CPAP machine, known as the “gold standard” for treating sleep apnea, is designed to regulate breathing while you sleep. However, it is notoriously regarded as unpleasant and fails for some people as a result.
a tube that connects your mouth and nose mask to your CPAP machine, which is about the size of a tissue box and has a motor. The device gently inhales air via the tube and into your airways as you sleep. To verify that the mask fits properly and that the right amount of air is being blasted through, a sleep expert may adjust the machine. “There are as many masks as there are shoes,” said Dr. Zinchuk, “and we can usually find the right one for each person.”
Modern CPAPs, according to Drs. Yaggi and Zinchuk, are “superior” because they include more comfortable masks, automatic pressure adjustment capabilities, built-in modems that transmit data to the doctor, and bi-directional capabilities that allow technicians to make adjustments remotely. Dr. Zinchuk claims that the device is still essentially the same. We’re working to remove anything that deters consumers from using it. The fundamental concept is nonetheless the same.

3. Setting the most recent CPAP recall in context
One matter that may be on people’s thoughts right now is the most recent recall of certain CPAP equipment. One CPAP manufacturer, Phillips Respironics, voluntarily recalled a number of ventilators, BiPAP, and CPAP devices in June 2021 due to potential health risks.
According to the Food and Drug Administration, the polyurethane foam with a polyester foundation used in these devices to reduce noise and vibration may decay (FDA). If this occurs, the person using the device could breathe in or swallow small pieces of black foam or other unseen materials. These issues might result in serious injury that could be life-threatening and need medical intervention to prevent irreparable harm.
Although these particles may potentially have detrimental or cancerous effects, the results of the testing show that emissions decrease after the device is used for the first time, hence the true threat remains unclear.
In light of this, some individuals may wonder how to determine their own particular dangers. The FDA claims that for certain patients, stopping use of the recalled or repaired device may be riskier than continuing to use it. Many people may not need to stop using their Respironics equipment, according to Dr. Zinchuk, especially those [with serious conditions] who need home ventilators for survival or those who have severe sleep apnea symptoms.
With your sleep expert, you must carefully weigh the benefits and drawbacks of continuing or stopping your CPAP therapy.
The FDA has a list of frequently asked questions about the recall, and Philips also offers a toll-free hotline with a Spanish language option at 877-907-7508.

4. CPAP substitutes are provided as therapeutic options.
There is good news for those who cannot tolerate the CPAP machine: Drs. Yaggi and Zinchuk state that because of improvements made to various sleep apnea medications, some patients may find them to be more successful (a sleep study may aid with this).
• The first line of defense for mild cases of OSA is lifestyle changes. This can include cutting down on or quitting alcohol use, losing weight, and quitting smoking.
• Oral appliances, which you place in your mouth to keep your airways open, may be prescribed by your doctor. They mimic retainers and work by pushing the jaw forward. When the user is laying down, they stop the tongue and other tissues from slipping back into the airway.
Upper airway exercises may help some patients finally stop using a CPAP machine by bolstering weak muscles that cause sleep apnea (such as those in the tongue and throat). Think of it as respiratory physical therapy, advises Dr. Yaggi.
- You may find it easier to breathe if you sleep on your side or stomach rather than your back. To help you keep a safe posture, there are several options at your disposal.
- Surgical procedures, including standard procedures on the palate (soft tissue at the back of your mouth and throat), as well as the nose, tongue, or other face organs, may be beneficial.
One effective CPAP replacement is the surgical implantation of the hypoglossal nerve stimulator, a pacemaker-sized device.
The device must be inserted via two incisions: one on the right chest wall and one in the neck, just below the jaw. Two electrodes, one attached to the area of the hypoglossal nerve that controls tongue propulsion forward and the other placed in the region between the rib muscles, are linked to a generator.
The device monitors breathing while stimulating the hypoglossal nerve. The muscles of the upper airway are able to keep the airway open by doing this. There’s no need for a mask.
You often stop breathing while you sleep if you have the dangerous sleep condition known as obstructive sleep apnea. Loud snoring and choking or gasping noises as you sleep are red flags.
According to estimates, around 30 million persons in the United States suffer with obstructive sleep apnea. Nearly one billion individuals may suffer from sleep apnea globally. Even Amy Poehler, an actress nominated for an Emmy, may suffer from sleep apnea.
Your life will likely be impacted by sleep apnea in some manner. You, your bed partner, or a different family member might be impacted. Here are six things to remember regarding sleep apnea.
Sleep apnea comes in two different forms.
Most often, obstructive sleep apnea occurs. It takes place when your muscles relax while you’re sleeping, resulting in soft tissue collapsing and blocking the airway. However, you are unable to breathe. Instability in your body’s respiratory control mechanism leads to central sleep apnea. During sleep, your body quits attempting to breathe.

Sleep apnea may happen to anybody, including very young children.
Even in newborns, central sleep apnea may develop. It can be a difficulty with development or the outcome of another illness. Pediatric obstructive sleep apnea is more frequent. Children’s huge tonsils and adenoids that obstruct the airway as they sleep are often the cause of sleep apnea.
Age-related increases in sleep apnea.
Ageing will continue to be a normal part of life up until the day when we get the means to halt it. Women are more prone to get sleep apnea after menopause, and the likelihood of having it rises with age. Additionally, the severity of sleep apnea often worsens gradually over time. Even while the prevalence of sleep apnea seems to stabilize around the age of 65, it is still possible to acquire the condition later in life.
Sleep apnea often goes undetected.
About 23.5 million adult Americans with sleep apnea are thought to go undiagnosed. Snoring is an indication of sleep apnea that far too many people ignore. Another research showed that women often underreport and underestimate the volume of their snoring. Women may also report symptoms like weariness or sleeplessness more often than men do.
Severe apnea that is left untreated might harm your health.
Sleep apnea may result in major medical issues if it is neglected and addressed. High blood pressure, heart disease, type 2 diabetes, stroke, and depression are some of these issues.
Lifestyle modifications may lessen the severity of sleep apnea.
Excess body weight is the main risk factor for sleep apnea. You may breathe more easily as you sleep if you are getting closer to a healthy weight. Additionally, you should abstain from alcohol use and smoking. Some individuals get sleep apnea more often when lying on their backs. Then positional treatment may be used to encourage side sleeping.
More to read: Know what this expert is saying about sleep apnea

